Patient Category 1: Cost-Sharing Assistance for Covered CGM: U.S. Patients who reside in the U.S., but not in Massachusetts, and whose commercial health insurance covers Dexcom G6 CGM as a prescription benefit, may use this program to receive assistance with cost-sharing amounts that they would otherwise pay out of pocket at the pharmacy. Eligible patients may use this voucher to obtain an instant rebate of. For Eligible Patients with Commercial Insurance: The Corlanor ® Tablet Copay Card reduces out-of-pocket (OOP) costs for Corlanor ®. Each patient is responsible for up to the first $20 of OOP costs. Lan tools for mac. The Corlanor ® Tablet Copay Card may then pay up to $160 per 30-day supply to cover OOP costs for Corlanor ® (up to $2,600 per year), including co-payments, co-insurance, and prescription deductible. An activated Co-pay Card together with a valid prescription for ELIQUIS at participating pharmacies may pay as little as $10 per 30-day supply (up to 74 tablets for the first fill and up to 60 tablets for all subsequent fills) for up to 24 months, subject to a maximum annual benefit of $3800. Other restrictions may apply.
The Amgen FIRST STEP™ Program is here to help eligible commercially insured patients pay for their out-of-pocket prescription costs, including deductible, co-insurance, and co-payment. If this is your first visit to our site, just click below to get started. If you're already registered, please login above. Microsoft for mac for free.
- Patient must be prescribed BLINCYTO® (blinatumomab), IMLYGIC® (talimogene laherparepvec), KANJINTI™ (trastuzumab-anns), KYPROLIS® (carfilzomib), MVASI™ (bevacizumab-awwb), Neulasta® (pegfilgrastim), Neulasta® Onpro®, NEUPOGEN® (filgrastim), Nplate® (romiplostim), Prolia® (denosumab), RIABNI™ (rituximab-arrx), Vectibix® (panitumumab), or XGEVA® (denosumab).
- Must have private commercial health insurance that covers medication costs for BLINCYTO®, IMLYGIC®, KANJINTI™, KYPROLIS®, MVASI™, Neulasta®, Neulasta® Onpro®, NEUPOGEN®, Nplate®, Prolia®, RIABNI™, Vectibix®, or XGEVA®.
- Must not be a participant in any federal-, state-, or government-funded healthcare program such as Medicare, Medicare Advantage, Medicare Part D, Medicaid, Medigap, Veterans Affairs (VA), the Department of Defense (DoD), or TriCare.
- May not seek reimbursement for value received from the Amgen FIRST STEP™ Program from any third-party payers, including flexible spending accounts or healthcare savings accounts. If at any time patients begin receiving coverage under any federal-, state-, or government-funded healthcare program, patients will no longer be eligible to participate in the Amgen FIRST STEP™ Program and must call 1-888-65-STEP1 (1-888-657-8371) Monday through Friday, 9 AM-8 PM EST to stop participation. Restrictions may apply. This is not health insurance. Program invalid where otherwise prohibited by law.
* Other restrictions apply. If you become aware that your health plan or pharmacy benefit manager does not allow the use of manufacturer co-pay support as part of your health plan design, you agree to comply with your obligations, if any, to disclose your use of the card to your insurer. Amgen reserves the right to revise or terminate this program, in whole or in part, without notice at any time.

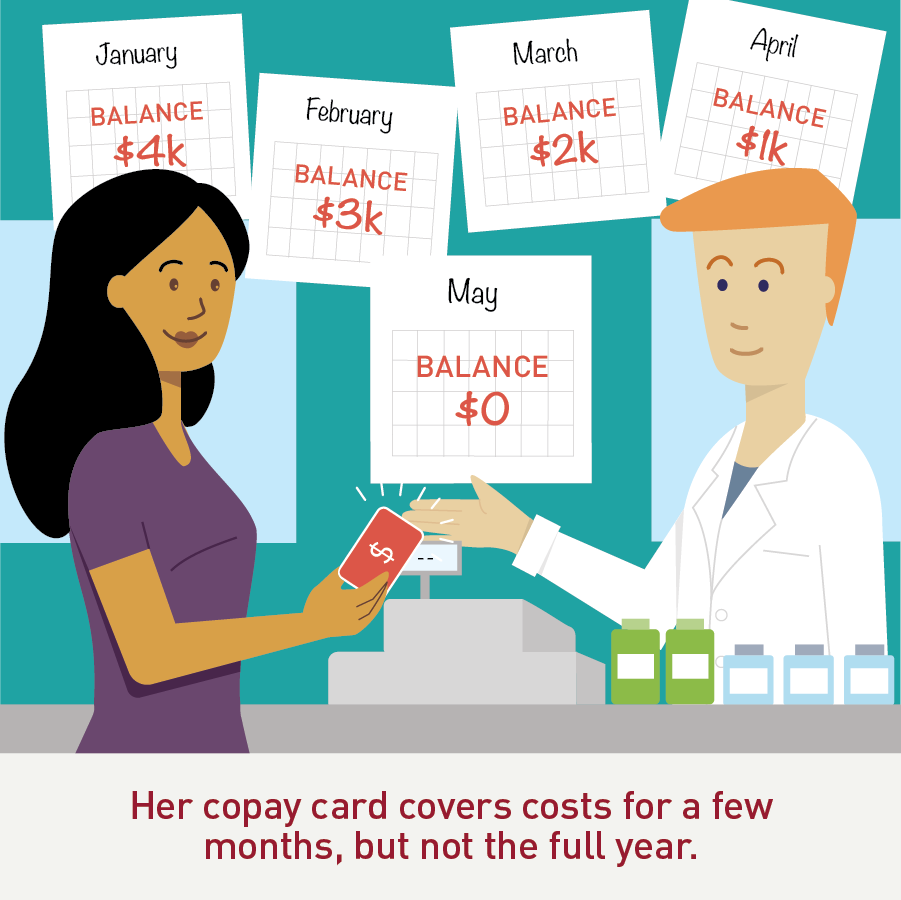
Patient First Copay Cards
- Program covers out-of-pocket medication costs for the Amgen product only. Program does not cover any other costs related to office visit or administration of the Amgen product. Patient is responsible for costs above the maximum benefit amounts detailed below.
- For Neulasta®, Neulasta® Onpro®, NEUPOGEN®, Nplate®, XGEVA®, Vectibix®, IMLYGIC®, and BLINCYTO®: no out-of-pocket cost for first dose or cycle; $5 out-of-pocket cost for subsequent dose or cycle; maximum benefit of $10,000 per patient per calendar year.
- For KANJINTI™, KYPROLIS®, MVASI™, and RIABNI™: no out-of-pocket cost for first dose or cycle; $5 out-of-pocket cost for subsequent dose or cycle; maximum benefit of $20,000 per patient per calendar year.
- For Prolia®: no out-of-pocket cost for first dose or cycle; $25 out-of-pocket cost for subsequent dose or cycle; maximum benefit of $1,500 per patient per calendar year.
- Ongoing activation of the Amgen FIRST STEP™ card is contingent on the submission of the required Explanation of Benefits (EOB) form by the healthcare provider's office within 45 days of use of the Amgen FIRST STEP™ card. Patients will be responsible for reimbursing the program for all amounts paid out if the EOB for the date of service is not received within 45 days.
Patient Copay Assistance Programs
Please see Full Prescribing Information, including Boxed WARNINGS, and Medication Guide for BLINCYTO®.
Please see Full Prescribing Information, including Boxed WARNINGS, for KANJINTI™.
Please see Full Prescribing Information, including Boxed WARNINGS, and Medication Guide for RIABNI™
Please see Full Prescribing Information, including Boxed WARNINGS, for Vectibix®.
